Midlife is typically a period marked by increasing professional pressures, complex family responsibilities, physical and hormonal changes, as well as the beginnings of anxiety about health and aging. These factors can contribute to the emergence of what is known as “midlife depression,” which can manifest in various forms. Some are traditional, such as persistent sadness and loss of passion, while others are more subtle and may be mistakenly attributed to exhaustion or aging.
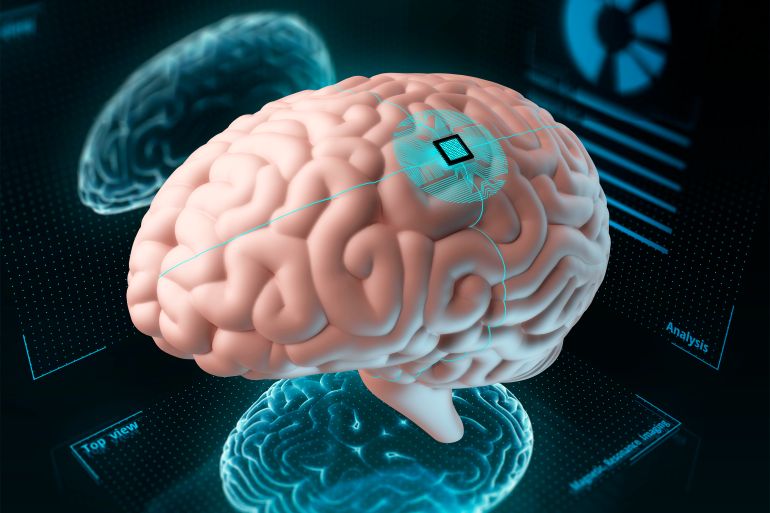
The danger of this type of depression lies in the fact that it not only affects mental health but is also linked to a decline in brain health and may contribute to an increased risk of dementia in later stages of life.
What is Midlife Depression?
Midlife depression is a psychological disorder that affects some individuals during the age range of 40 to 60. This disorder can take the form of clear clinical depression or may present with partial depressive symptoms that do not meet the full criteria for medical diagnosis but profoundly affect the quality of life.
This type of depression does not differ in its biological basis from depression at other life stages, but it is distinguished by its specific context. It often intersects with feelings of lost meaning, evaluation of life achievements, or fear of health and professional decline.
Causes of Midlife Depression
There are numerous reasons that may contribute to the onset of depression during this phase. Psychologically, a person may feel they have not achieved what they aspired to or that they are trapped in a life they did not desire.
From a social perspective, this stage may coincide with children leaving home, caring for elderly parents, or accumulated financial pressures. Biologically, hormonal and neurological changes occur that can affect mood and emotional regulation, in addition to the accumulation of health risk factors such as high blood pressure or diabetes, which in turn affect brain health.

The Relationship Between Midlife Depression and Dementia
Some studies, which have followed tens of thousands of people over decades, indicate a strong association between the appearance of specific depressive symptoms in midlife and an increased risk of developing dementia in later stages of life by approximately 50%.
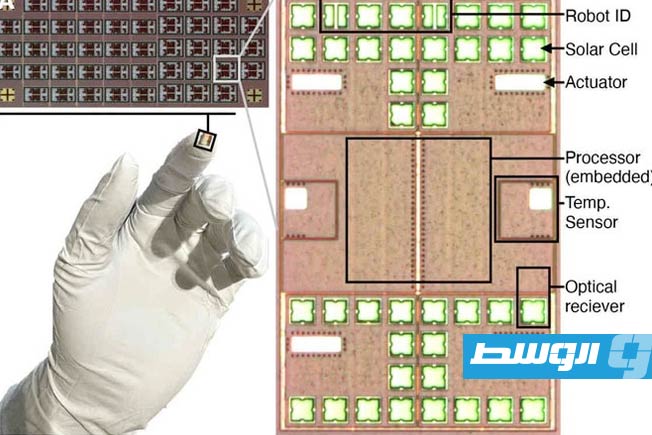
These studies tracked the impact of midlife depression symptoms on cognitive decline and brain health, showing that some partial depressive symptoms, even those that do not meet the full criteria for clinical depression, have a higher predictive value for dementia risk compared to others. The researchers concluded by identifying six key symptoms that were notably recurrent among individuals who later developed dementia:
First: Loss of Pleasure or Interest in Things That Were Previously a Source of Happiness
This symptom is an indicator of dysfunction in the neural circuits responsible for reward, particularly those associated with dopamine in areas such as the prefrontal cortex and the limbic system. These regions not only regulate emotions but also play a central role in memory, attention, and decision-making.
When their function is impaired in midlife, it may reflect the beginning of a decline in the efficiency of the very neural networks that are later affected in dementia. This makes the loss of pleasure not merely a psychological symptom but a potential marker of early brain changes associated with an increased risk of cognitive decline.
Second: Apathy or Reduced Motivation
This symptom is not limited to a transient feeling of laziness or fatigue but reflects a clear decline in the ability to initiate, make decisions, and engage in social and daily activities. These functions are closely linked to the integrity of the frontal lobe and the neural networks responsible for planning, organization, and behavioral control—some of the first areas affected in certain types of dementia, especially vascular dementia and frontotemporal dementia. Therefore, the emergence of apathy in midlife may be an early sign of dysfunction in these neural circuits, explaining its association with an increased risk of later cognitive decline.
Third: Chronic Fatigue and Loss of Energy
This symptom is not limited to a physical